How to Get Rid of Vaginal Bumps: Your Ultimate Guide

Discover how to get rid of vaginal bumps effectively and confidently! Experiencing bumps in the vaginal area can be a source of concern for many, but understanding their causes and appropriate remedies can bring immense relief. This comprehensive guide aims to demystify these common occurrences, offering clear, actionable advice to help you achieve a smooth and comfortable intimate area.
Understanding Vaginal Bumps: What Are They?
Vaginal bumps, often referred to as vulvar bumps or labial bumps, are a common phenomenon that can appear on the external genitalia. They can range in size, texture, and appearance, and their presence can be unsettling. It’s important to remember that not all vaginal bumps are a cause for alarm, and many are benign and temporary. However, understanding the potential culprits is the first step towards effective management and knowing how to get rid of vaginal bumps.
Common Causes of Vaginal Bumps
The skin in the vulvar region is sensitive and prone to various conditions that can manifest as bumps. Here are some of the most frequent causes:
- Ingrown Hairs: This is perhaps the most common culprit, especially after shaving, waxing, or epilating. When a hair follicle becomes blocked or a hair grows back into the skin, it can cause a red, inflamed bump, sometimes with a small pustule. These can be itchy and tender.
- Folliculitis: Similar to ingrown hairs, folliculitis is an inflammation or infection of the hair follicles. It can be caused by bacteria, fungi, or even irritation from tight clothing. Folliculitis bumps often resemble small pimples and can be itchy or painful.
- Cysts:
- Bartholin’s Cysts: These form when the Bartholin’s glands, located on either side of the vaginal opening, become blocked. They can be small and asymptomatic or grow larger, causing discomfort or pain, especially when walking or during intercourse. If infected, they can form an abscess.
- Epidermoid Cysts (Sebaceous Cysts): These are non-cancerous lumps that grow under the skin. They are caused by a buildup of keratin, a protein found in skin cells. They are usually firm and can vary in size.
- Sexually Transmitted Infections (STIs): Certain STIs can present as bumps or sores.
- Genital Warts (HPV): Caused by the human papillomavirus, these can appear as small, flesh-colored or grayish bumps, often with a cauliflower-like appearance. They are typically painless but can spread.
- Genital Herpes: This viral infection can cause painful blisters or sores that eventually break open and crust over. The initial outbreak can be accompanied by flu-like symptoms.
- Syphilis: In its primary stage, syphilis can manifest as a painless sore called a chancre. This sore can appear on the genitals, anus, or mouth.
- Molluscum Contagiosum: This is a viral skin infection that causes small, firm, dome-shaped bumps with a central dimple. They are usually painless but can be itchy and spread through direct contact.
- Skin Tags: These are small, soft, fleshy growths that hang off the skin. They are benign and often occur in areas where skin rubs against skin or clothing.
- Acne: While more common on the face, acne can also occur in the pubic area, leading to pimples and blackheads.
- Allergic Reactions or Irritation: Contact with certain soaps, detergents, lubricants, or latex can cause an allergic reaction or irritation, leading to redness, itching, and bumps.
How to Get Rid of Vaginal Bumps: Effective Solutions
Now that we’ve explored the potential causes, let’s delve into how to get rid of vaginal bumps and manage them effectively. The approach will depend on the underlying cause.
Home Remedies and Self-Care for Common Bumps
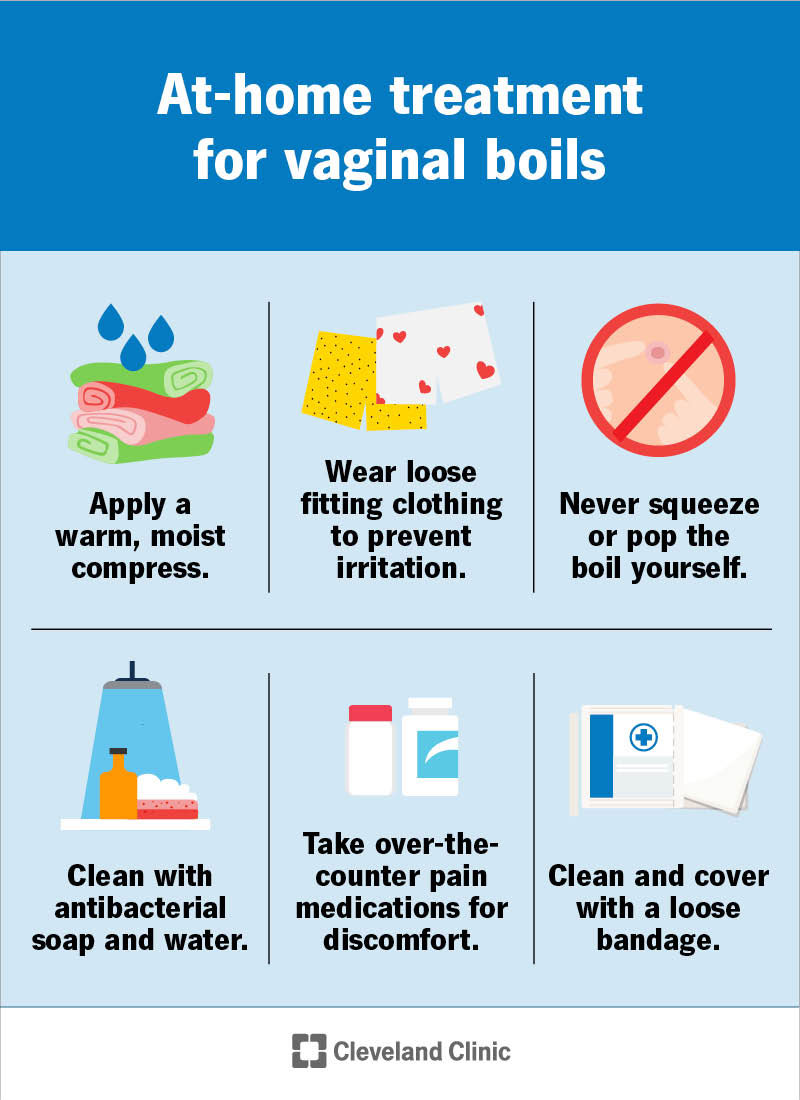
For minor issues like ingrown hairs, folliculitis, or mild irritation, several home remedies can provide relief and encourage healing.
Managing Ingrown Hairs and Folliculitis
- Gentle Exfoliation: Regular, gentle exfoliation can help prevent ingrown hairs by removing dead skin cells that can trap hairs. Use a soft washcloth or a mild exfoliating scrub a few times a week. Avoid harsh scrubbing, which can worsen irritation.
- Warm Compresses: Applying a warm, moist compress to the affected area for 10-15 minutes, several times a day, can help reduce inflammation, soften the skin, and encourage any trapped hairs to surface.
- Avoid Picking or Squeezing: Resist the urge to pick at or squeeze ingrown hairs or folliculitis bumps. This can lead to infection, scarring, and increased inflammation.
- Loose-Fitting Clothing: Opt for breathable, loose-fitting cotton underwear and clothing to minimize friction and allow the skin to breathe.
- Antibacterial Washes: Over-the-counter antibacterial washes can be helpful in preventing and treating folliculitis, especially if it’s caused by bacteria. Look for ingredients like benzoyl peroxide or chlorhexidine.
- Tea Tree Oil: Diluted tea tree oil has natural antiseptic and anti-inflammatory properties. Mix a few drops with a carrier oil like coconut oil and apply to the affected area with a cotton swab. Always do a patch test first to ensure no adverse reaction.
Soothing Irritated Skin
- Cool Compresses: If the bumps are red and itchy due to irritation, a cool compress can provide soothing relief.
- Gentle Cleansing: Use a mild, fragrance-free soap or a specialized intimate wash to clean the vulvar area. Avoid harsh chemicals or perfumed products.
- Aloe Vera Gel: Pure aloe vera gel can help calm inflamed skin and promote healing.
When to Seek Medical Advice: Crucial Steps
While many vaginal bumps are harmless, it’s crucial to know when to consult a healthcare professional. If you experience any of the following, seek medical attention promptly:
- Severe Pain or Discomfort: If the bumps are causing significant pain, making it difficult to walk or sit.
- Rapid Growth or Change: If a bump is growing rapidly, changing in appearance, or bleeding without apparent cause.
- Signs of Infection: Fever, chills, increased redness, swelling, warmth, or pus discharge.
- Suspicion of STIs: Any new sores, blisters, or unusual discharge, especially if you’ve had unprotected sex.
- Persistent Bumps: If bumps don’t improve with home care after a week or two, or if they keep recurring.
- Lumps That Feel Hard or Unusual: Any lump that feels significantly different from typical skin bumps.
Medical Treatments for Vaginal Bumps
A healthcare provider can accurately diagnose the cause of your vaginal bumps and recommend appropriate medical treatments.
- Antibiotics or Antivirals: If the bumps are due to a bacterial or viral infection (like folliculitis, herpes, or syphilis), your doctor will prescribe appropriate medication.
- Topical Treatments: For conditions like acne or mild folliculitis, your doctor might recommend prescription-strength topical creams or ointments containing retinoids, antibiotics, or anti-inflammatories.
- Cyst Drainage or Removal: For larger or symptomatic Bartholin’s cysts or epidermoid cysts, your doctor may recommend drainage or surgical removal.
- Cryotherapy or Laser Treatment: Genital warts caused by HPV can be treated with cryotherapy (freezing), laser treatment, or topical medications.
- Steroid Injections: In some cases of severe inflammation, steroid injections might be used.
Prevention is Key: Avoiding Future Vaginal Bumps
Once you’ve successfully addressed existing vaginal bumps, focusing on prevention can significantly reduce the likelihood of them returning.
Smart Hair Removal Practices
- Exfoliate Before and After: Gentle exfoliation before hair removal can help lift hairs, and continued exfoliation afterward can prevent them from becoming trapped.
- Use a Sharp, Clean Razor: Dull razors can cause irritation and nicks. Always use a sharp, clean razor and shave in the direction of hair growth.
- Shaving Cream or Gel: Always use a lubricating shaving cream or gel to create a smooth surface and reduce friction.
- Consider Alternatives: If shaving consistently leads to ingrown hairs, explore other hair removal methods like waxing (done by a professional), epilating, or laser hair removal.
- Allow Skin to Breathe: After hair removal, avoid tight clothing for a few hours to allow the skin to recover.
Maintaining Good Hygiene
- Gentle Cleansing: Wash the vulvar area daily with warm water and a mild, fragrance-free soap. Avoid douching, as it can disrupt the natural balance of bacteria.
- Dry Thoroughly: After washing, gently pat the area dry to prevent moisture buildup, which can encourage bacterial or fungal growth.
- Change Underwear Regularly: Change underwear daily, or more often if you sweat heavily.
Choosing the Right Products
- Hypoallergenic and Fragrance-Free: Opt for intimate washes, lubricants, and laundry detergents that are hypoallergenic and fragrance-free to minimize the risk of irritation and allergic reactions.
- Breathable Fabrics: Choose cotton underwear and clothing made from natural, breathable fabrics.
Busting Myths About Vaginal Bumps
It’s common to have misconceptions about vaginal bumps. Let’s address a few:
- Myth: All vaginal bumps are STIs.
- Fact: While some STIs can cause bumps, many other benign conditions can also lead to them. Accurate diagnosis is crucial.
- Myth: You can pop any vaginal bump like a pimple.
- Fact: This can worsen infections, cause scarring, and is not recommended for most types of vaginal bumps.
- Myth: Vaginal bumps are always a sign of poor hygiene.
- Fact: While good hygiene is important, bumps can occur due to various factors, including genetics, hormones, and hair removal practices, even with excellent hygiene.
Frequently Asked Questions About Vaginal Bumps
Q1: How can I tell if a vaginal bump is serious?
A1: If a bump is causing severe pain, growing rapidly, showing signs of infection (fever, pus), or if you suspect an STI, it’s important to see a doctor.
Q2: Are ingrown hairs common in the vaginal area?
A2: Yes, ingrown hairs are very common, especially after hair removal methods like shaving or waxing.
Q3: Can I use acne medication on vaginal bumps?
A3: It’s generally not recommended to use over-the-counter acne medications without consulting a doctor, as the skin in the vaginal area is sensitive and may react differently.
Q4: How long does it take for a vaginal bump to go away?
A4: The healing time varies greatly depending on the cause. Ingrown hairs might resolve in a few days to a week, while cysts or infections may take longer and require medical treatment.
Q5: Is it safe to have sex if I have vaginal bumps?
A5: This depends on the cause. If the bumps are due to an STI or are painful, it’s best to avoid sexual activity until they have healed or been treated. Consult your doctor for personalized advice.
Conclusion: Empowering Yourself with Knowledge
Understanding how to get rid of vaginal bumps is about more than just eliminating them; it’s about empowering yourself with knowledge and taking proactive steps for your intimate health. By recognizing the common causes, employing effective home care strategies, and knowing when to seek professional medical advice, you can navigate this concern with confidence. Remember, your body is unique, and open communication with your healthcare provider is always the best path to ensuring your well-being.
If you found this guide helpful, please share it with others who might benefit! Your journey to a comfortable and healthy intimate area is within reach.






You may also like

How to Clear Pregnancy Acne: Your Radiant Glow Guide

How to Get Rid of Baby Pimples: A Gentle Guide to Clearer Skin

How to Help Acne During Pregnancy: Your Radiant Skin Guide
Recent Posts
- How to Clear Pregnancy Acne: Your Radiant Glow Guide
- How to Get Rid of Baby Pimples: A Gentle Guide to Clearer Skin
- How to Help Acne During Pregnancy: Your Radiant Skin Guide
- What is Good for Pimple Scars? Unveiling Radiant Skin!
- What Helps With Pimple Scars: Unveiling Your Path to Flawless Skin!
- How to Get Rid of Scarred Pimples: Unlocking Radiant Skin!
Leave a Reply